Abstract
Background Primary breast diffuse large B-cell lymphoma (DLBCL) has poor outcomes with frequent extranodal failures, particularly in the central nervous system (CNS). Recent studies have reported that cell-of-origin (COO), BCL2/MYC dual expression (DE), and MYC and BCL2 and/or BCL6 rearrangements, so-called double hit (DH) and triple hit, are associated with a high risk of CNS progression in DLBCL; however, the impact of these biologic markers in primary breast DLBCL on CNS progression remains unknown.
Methods CNS progression was analyzed in newly diagnosed primary breast DLBCL patients identified from 2 sources: the prospective study of the Consortium for Improving Survival of Lymphoma (CISL) study group conducted from January 2012 to July 2017, and the retrospective cohort included patients who were treated outside clinical trial at any CISL institutions between January 2012 and December 2020. Briefly, the prospective study (Yhim HY et al. Cancers 2020;12:2192) included 33 patients (20-75 years of age) with primary breast DLBCL, and treatment consisted of 6 cycles of rituximab plus cyclophosphamide, doxorubicin, vincristine, and prednisone (R-CHOP) and 4 doses of intrathecal (IT) methotrexate (MTX) at a 3-week interval. The eligibility criteria for the retrospective cohort were virtually the same as the prospective cohort, except for no age limit. 26 patients were screened, 6 of whom were excluded because of incomplete data (n=4) and secondary breast DLBCL (n=2). Thus, the retrospective cohort included 20 patients treated with 6 cycles of R-CHOP ± radiotherapy. CNS prophylaxis was not considered for eligibility in this cohort but was done in 17 patients (4-6 doses of IT MTX [n=14] and systemic high-dose MTX [n=3]). Expert hematopathologists centrally assessed COO and DE status. COO was determined using the Hans algorithm. MYC (≥40%) and BCL2 (≥50%) protein expressions were used to assign DE. Fluorescence in situ hybridization testing was used to determine DH lymphoma. The risk of CNS progression was estimated using the cumulative incidence method. The impact of variables of interest on CNS progression was assessed using a multivariable Cox model.
Results We identified 53 patients from 2 data sources. The median age was 55 years (range, 29-78), and all were female. Most patients had unilateral (n=50, 94%), localized-stage (n=48, 91%), and ECOG performance status ≤1 (n=51, 95%). Serum LDH level was elevated in 14 (26%). Hence, IPI and CNS-IPI risks were mainly low (n=45, 85%). No patients had CNS disease at diagnosis.
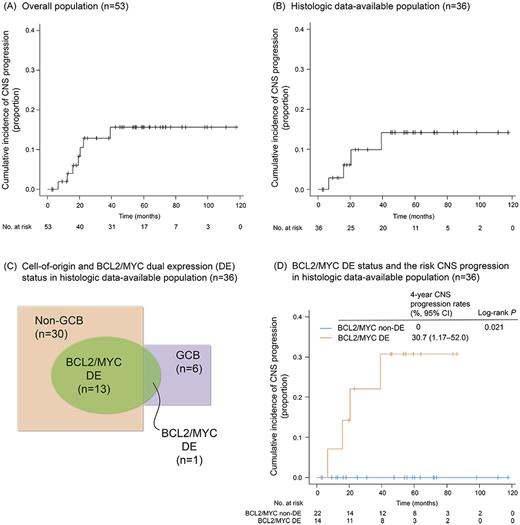
With a median follow-up of 58.8 months (IQR, 30.3-72.9), 7 patients developed CNS progression (parenchymal only, n=4; leptomeningeal only, n=2; parenchymal and leptomeningeal, n=1). The 4-year cumulative incidence of CNS progression was 15.6% (95% CI, 6.7-27.9; Fig A). The Cox analysis revealed bilateral breast involvement (HR, 9.39; 95% CI, 1.69-52.18) was an independent factor for CNS progression in this population.
Of the 53 patients, 36 were selected as a histologic data-available population because of a lack of diagnostic materials for COO and DE in 17 patients. Baseline characteristics of the histologic data-available population (n=36) were similar to the overall population (n=53). In the 36 patients with histologic data available, 4 patients had CNS progression (parenchymal only, n=2; leptomeningeal only, n=1; parenchymal and leptomeningeal, n=1), and the 4-year CNS progression rate was 14.2% (95% CI, 0.4-26.3; Fig B). According to the Hans algorithm, 30 (83%) and 6 (17%) were classified as having non-GCB and GCB, respectively. 14 patients (39%) had BCL2/MYC DE, of whom 13 were non-GCB subtype (Fig C). The CNS progression rate of non-GCB did not differ significantly from that of the GCB subtype (4-year, 17.4% vs. 0%; p=0.326), but BCL2/MYC DE had a higher risk of CNS progression than non-DE (4-year, 30.7% vs. 0%, p=0.021; Fig D). 20 patients had sufficient tissue to test DH status, but no DH cases were identified. The multivariable Cox analysis of these 36 patients showed bilateral involvement (HR, 3.73; 95% CI, 1.28-10.86) and BCL2/MYC DE (HR, 2.42×104; 95% CI, 0.51×104-10.60×104) were independent predictors for CNS progression.
Conclusion Our data suggested that bilateral breast involvement and BCL2/MYC DE were independent risk factors for CNS events in patients with primary breast DLBCL.
Disclosures
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.